Fact Sheet (PDF) | Facts Card: Image or PDF | Harm-reduction information: Image or PDF | Links | Resources
AKA: Benzos, tranx, sleepers,
downers. Specific drugs are referred to by their chemical name, brand name,
and some have got slang names. Brand names vary around the world adding to
confusion so for example the drug Diazepam is known by the brand name Valium in
the UK, but is also known internationally by many other trade names including
Mano, Anxol, Placidox and many other.
|
Name |
Brand |
Slang |
Notes |
|
ALPRAZOLAM |
Xanax |
Xs, Xans |
Not
an NHS stock drug; Available
in UK on private prescription |
|
CHLORDIAZEPOXIDE |
Librium |
|
Primarily used in in alcohol detox |
|
DIAZEPAM |
Valium |
Vallies, blues |
Widely prescribed for
daytime anxiety |
|
FLUNITRAZEPAM |
Rohypnol |
Rohies, rufies |
Strong associations with drink spiking |
|
NITRAZEPAM |
Mogadon |
Moggies |
|
|
TEMAZEPAM |
Normison |
temazies, jellies,
eggs |
Used to be widely
injected |
|
ETIZOLAM |
|
|
Widely available as
an illicit benzo; |
For
a number of years an additional route for sourcing benzodiazepines was the
overseas prescription market. A number of websites, located outside the UK,
would offer an online “consultation” with a “doctor” and then a “prescription”
would be issued and “benzos” supplied. In practice the variability of the
supplied pills was massive and many of these websites have been shut down.
This approach has been nominally successful with a significant and sustained
drop in benzodiazepine prescribing.
However as the charts below show in the first instance the drop in Benzo
prescribing represented in part simply a shift from one sedating drug to
another. Initially the Z drugs started to get used in place of Benzos. They
were initially not controlled drugs and not perceived to be addictive.
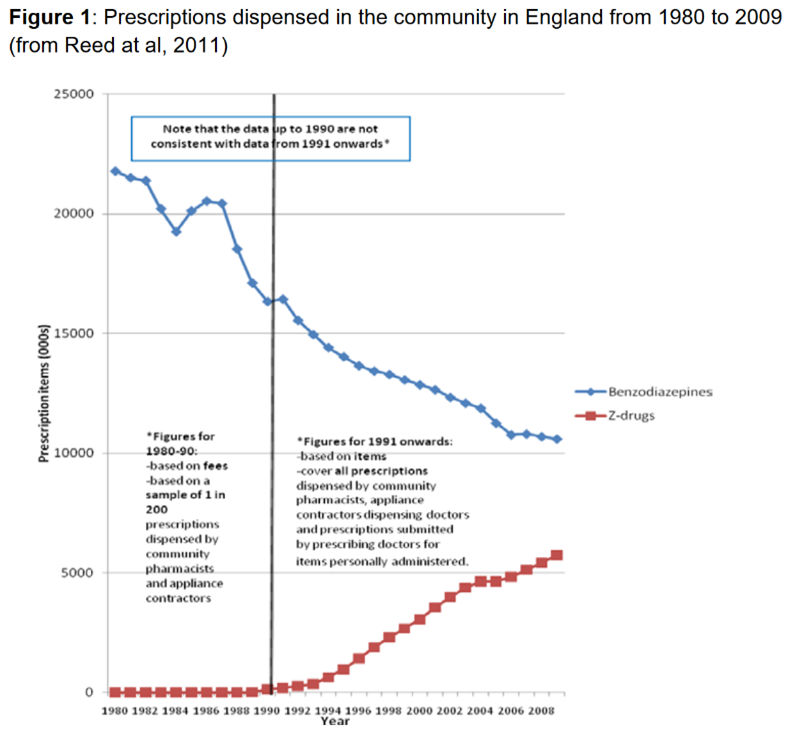
Subsequently
even though benzos and related drugs became harder to get through legitimate
routes, the massive growth of legal benzos as part of the NPS scene and their
subsequent consolidation as an illicit street drug has meant that in some areas
illicit benzos are more of an issue now than leaked prescribed benzos.
Most are distributed as tablets or capsules. A small number of unregulated
compounds are sold as powders. Benzos may also turn up as a cut in other drugs,
especially heroin. Overdoses linked to “strong heroin” or “fentanyl” in heroin
often turn out to be benzos cuts.
A few also come in preparations for injection, such as Valium ampoules, which
command a higher street value.
Different brands of drug will vary from company to company. Tablets will vary
in colour, shape and markings. The
appearance of each drug varies widely so visual pill identification is
difficult.
While it’s no guarantee that pills that
are sold in intact foil strips with UK specific labelling are less likely to be
counterfeit.
Drugs supplied loose, or in overseas packaging are more likely to be
counterfeit.
 The mainstay of the street benzodiazepine market has, since the 80s, been diazepam. The most widespread and
popular strength, a 10mg tablet, is often a scored blue tablet. As a result,
people manufacturing tablets to sell as diazepam invariably produce a blue tablet. These
can vary massively in consistency and strength. Some are merely white powders,
dyed blue and compressed into tablets.
The mainstay of the street benzodiazepine market has, since the 80s, been diazepam. The most widespread and
popular strength, a 10mg tablet, is often a scored blue tablet. As a result,
people manufacturing tablets to sell as diazepam invariably produce a blue tablet. These
can vary massively in consistency and strength. Some are merely white powders,
dyed blue and compressed into tablets.
Alprazolam (Xanax) has become
increasingly popular in the UK. As it is not widely prescribed on the NHS,
Alprazolam sold in the UK may be from private prescriptions, overseas
pharmacies, or grey-market tablets batched from raw alprazolam powder. These
can vary greatly in strength and consistency. Alprazolam is typically sold as
white, scored bars with XANAX printed on them.
Cost: At a street level, benzodiazepines have
a very low value, typically around 50p per tablet. Ampoules can cost £5 and are
rarely available now. Depending on dose and quantity stronger pills like Xanax
can sell for between £1-5 depending on claimed dose.
Quality: If pills are genuine pharmacy product, quality
is assured. However, it is impossible to correctly identify loose drugs in this
family by eye, let alone assay the strength, so mistakes in strength and name are
frequent amongst those purchasing non-medical products.
With so many imported, fake, unlicensed
and novel products entering the market, the risks with non-pharmacy products
will increase. Products could contain something stronger, weaker or different.
It is possible to send pills to a
service like WEDINOS https://www.wedinos.org/
to find out which drug(s) are present in
a batch. Whilst useful to identify compounds, WEDINOS doesn’t share information
about dose or level of different compounds so is of limited benefit from a harm
reduction or dependency/taper point of view. While the service may indicate a
blue pill contains diazepam and etizolam it won’t say how many milligrams of
each drug are present.
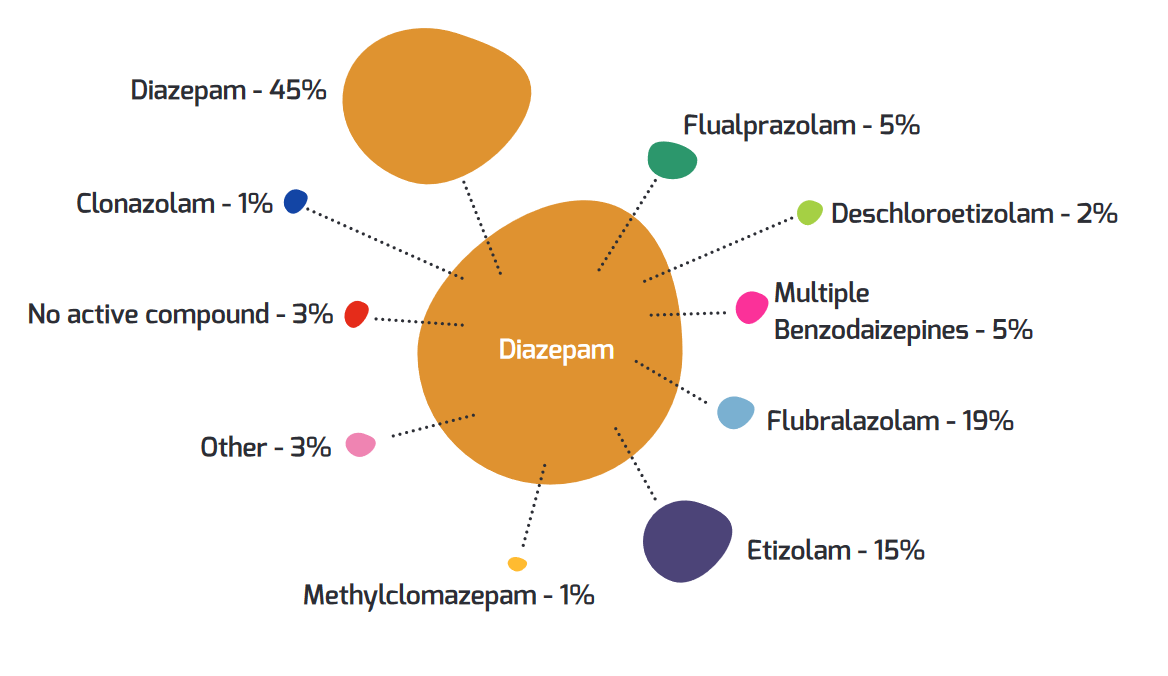
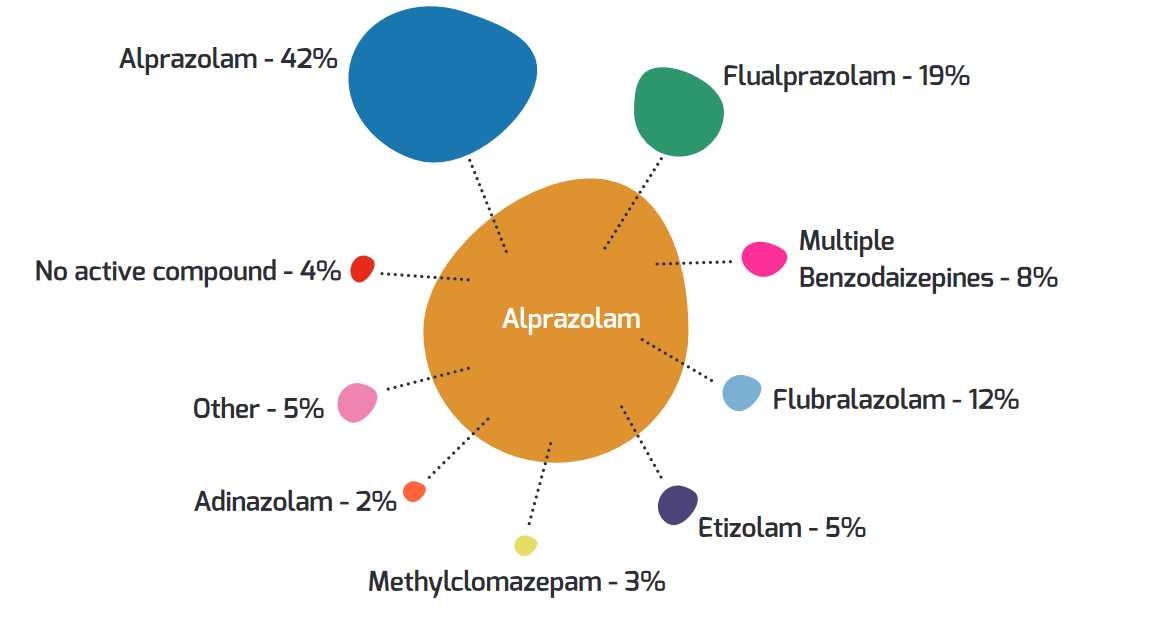
[Source
WEDINOS Annual Report 2021-22]
Methods of
Use: Tablets are designed for oral use,
though some users crush and inject tablets. As diazepam has very poor
solubility in water this is damaging and not very effective. Diazepam itself is
relatively short acting; on ingestion it is metabolised in to a long-acting
metabolite nor-diazepam so the risk is that people need to redose more
frequently if taking via routes other than swallowing. There are some reports
of snorting, especially of novel, unregulated benzodiazepines.
Detection: Immuno-assay (urine
test) kits can detect a range of benzodiazepine metabolites and related
compounds. They are not sensitive for all benzos. This varies according to:
High dose, lower potency, longer acting benzos structurally closer to diazepam
will show up on most tests.
Shorter acting drugs, highly potent drugs and drugs that produce other
metabolites may not show up.
In situations where a person is adamant that they are using a benzo-type drug
but the urine tests negative, it could be that this specific drug at this
specific dose doesn’t show up on this specific urine test. Double checking via
a different brand of test or, ideally, via GC/MS would be a better option.
Some drugs, like GHB and Barbiturates, are GABA agonists (mimics).
Benzodiazepines are not thought to be full GABA mimics. Instead,
benzodiazepines bind to Benzodiazepine Receptors (BZ receptors) and appear to increase
the regulatory effect of GABA. They need GABA, or a GABA-mimic present to work.
Specific benzodiazepines are believed to be more active at different BZ
receptors. This may result in different benzos having greater or lesser
sleep-inducing, muscle relaxing or anxiolytic effects.
Reasons
for Use: Benzodiazepines are still
used medically for a range of conditions including:
Anti-convulsants anti-anxiety (anxiolytic) sleep-inducing (hypnotic)
muscle
relaxant amnesiac alcohol
detoxification
Non-medical use follows similar
patterns, self-medicating for a range of conditions including anxiety and
insomnia. They are also popular as “come-down” drugs following use of
stimulants. The sense of intoxication when used with opiates or alcohol is
greater, so these combinations are widely used. This brings a bigger risk of
overdose.
Benzos can help people not remember or remember without emotion making them
popular choices for managing traumatic memories. They can create a sense of
detachment, depersonalisation or “derealization,” making the real world feel
less present or intrusive.
The sense of calm, detachment, well-being and relaxation from benzos makes them
highly sought after amongst people experiencing negative mental health
symptoms.
Very strong benzos such as Flubromazolam are believed to be 40x the strength of
Diazepam. If a pill contained 1mg of flubromazolam, this would be the
equivalent of 40mg of diazepam (i.e. 4 x 10mg diazepam.)
In street settings upper dose range will vary massively according to tolerance.
Some people will build up dose tolerance far above therapeutic dose range.
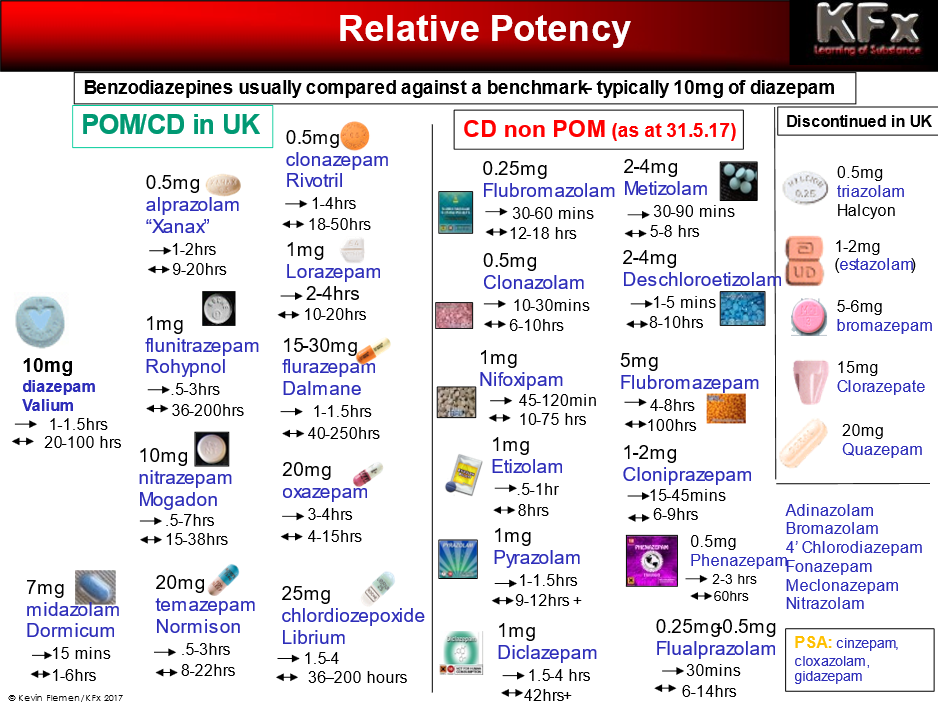
In the diagram above the first arrow is
an indication of onset and the second is the duration of effect. Slow-onset
benzodiazepines increase the risk that a person will re-dose before drugs have
started working properly.
Some benzodiazepines produce active
metabolites, with very long half-lives. Some can last 100-200 hours or longer.
These long-acting drugs increase the risk of building up tolerance, and that
any later drug use will be taking place on top of residual benzodiazepines. For
example, diazepam used on Sunday will probably still be in the system on
Tuesday or Wednesday. This means that alcohol use on these days is effectively
taking place on top of benzodiazepines.
Indicators of Use: Aside from
physical evidence such as packaging, there are few markers for benzo use.
Illicit fake diazepam can cause blue staining to lips and tongue. Otherwise
indicators are simply drowsiness, relaxation and possibly appearing drunk, but
without the smell of alcohol.
Whilst older benzos will show up on urine tests,
some of the newer products such as Etizolam are sufficiently structurally
different so won’t show up on some urine tests.
Effects: Benzos can cause physical
relaxation, reduce stress and anxiety. Users may become drowsy or fall asleep.
They can have a big impact on memory, causing amnesia. They can also cause
slurred speech, clumsiness, and confusion. People report euphoria and some
people find benzos disinhibiting, in the same way that alcohol is. Some users
gain a feeling of invulnerability or invisibility when using benzodiazepines.
They may find this useful when, for example, shoplifting. Some users experience
depression and, paradoxically, a few users become over-excited or violent.
Dependency: When used within a supervised
medical regime, benzodiazepines should not be used for extensive periods as
tolerance develops rapidly and withdrawal can be an unpleasant and, in some
cases, dangerous process. After a few weeks, and certainly within a few months,
their therapeutic value decreases. The person using them will still experience
effects, some of which are placebo and some of which are relief from withdrawal
symptoms.
For physically dependent users, abrupt
withdrawal can cause a range of symptoms. These can range from the mild to the
life threatening. Several factors including underlying physical and mental
health conditions, duration of use, dose and expectations can influence the
experience of withdrawal.
Withdrawal from Benzodiazepines should
always be tapered rather than done suddenly.
Where there is evidence of high doses,
long-term use, or where the person has a history of illness such as epilepsy,
withdrawal should be done under medical supervision. IT IS POSSIBLE TO DIE DUE
TO SEVERE BENZODIAZEPINE WITHDRAWAL.
The approach had great utility where
people were on NHS dose ranges of up to 30mg of diazepam and could see
reductions completed within 30-60 weeks.
The situation is now far more complex and at present there is a lack of
effective treatment for people dependent on non-prescribed benzos.
The problem has a number of dimensions:
There is always going to be a need for
psychosocial support during and after benzo treatment. However mental health
teams will typically not see people while they are still receiving drug
treatment or perceived to be “still using” meaning that it will fall to drug
services to address underlying issues such as anxiety or traumatic memories
until other services are prepared to engage.
- have street tablets assessed for strength and composition
- calculate a dose equivalent and
prescribe to that
- do a taper at a pace comfortable for
and in agreement with the person using
- engage from the start with
psychosocial services
- where customers are using opiates,
alcohol and benzos problematically, undertake stabilisation prescribing on the
benzos and address alcohol and opiate use sequentially before addressing the
benzos.
However, in combination with other
drugs, especially alcohol and opiates, the risk of fatal overdose is far
higher. A large number of dependent drinkers and people on opiate substitution
therapy are also prescribed diazepam, increasing risk of dangerous polydrug
use.
Opiate antagonists are not useful in benzo only or benzo/alcohol overdoses.
Where benzos are used with heroin, use of naloxone is useful as it can restore
respiration suppressed by opiates.
It is therefore important to stress the importance of calling an ambulance to
all overdoses in case it is a benzo-primary overdose, not an opiate-primary.
There is a blocker for benzo which can be used in OD but as it can cause
convulsions, is less suitable for peer distribution like naloxone.
Legal Status:
Most Benzodiazepines are class C drugs and nearly all are Schedule 4i drugs,
meaning that they can only be supplied, produced and possessed by those
authorised to do so. The law on Schedule 4 drugs changed in 2002; prior to that
it was not an offence to possess benzodiazepines without prescription.
Temazepam and Flunitrazepam (Rohypnol)
were reschedule Schedule 3 drugs.
Formerly unregulated benzodiazepines
(such as etizolam) were brought under the MoDA in May 2017. The benzos were
added as a list rather than via an “analogue” clause which means that there is
scope for developing new benzos that will not be covered by the MoDA. Any such
emergent benzos will automatically be covered by the Psychoactive Substances
Act 2016.
Other Information: Benzodiazepines were
introduced and have largely supplanted the BARBITURATE group of drugs, which
were widely prescribed and widely misused in the seventies. Benzos were seen as
preferential to barbiturates as the risks of overdose, dependence and
side-effects were thought to be less. They were massively overprescribed. As
awareness grew of the risks of tolerance and dependency this overprescribing
has been reduced but there are still a huge number of people inappropriately
prescribed. Unfortunately, in a knee-jerk reaction to this over-prescribing
some doctors are removing people from prescribed medication with fast tapers
and a lack of additional support. Some of these benzo patients get referred to
drug services. Increasing numbers end up getting stronger benzos through other
routes so the well-intentioned restriction in prescribing is creating a bigger
problem by pushing people on to the unregulated street market.
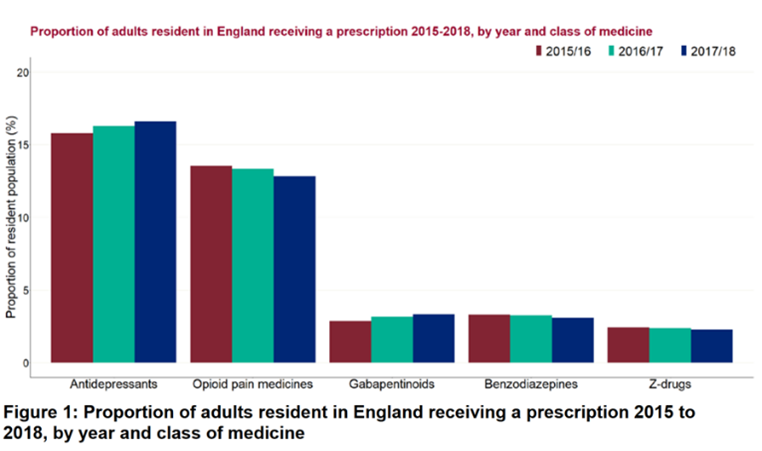
Prescribers are very aware of benzodiazepine over prescribing, and in many
areas greater care is now taken to reduce and monitor prescribing. However, a number
of other drugs have been less closely monitored and have increased in
popularity.
Initially, the “Z-Drugs” (Zopiclone, Zimovane, Zaleplon) increased and of
course started to be misused. The law in relation to some of these has now been
tightened and they are now Controlled Drugs.
More recently, Gabapentin and Pregabalin have emerged as the latest of the
sedating drugs to shift from medical to non-medical settings. Although not
benzodiazepines, they work in the same parts of the brain, with similar risks
in terms of tolerance, dependency and overdose.
Whilst the use of prescribed diazepam is undoubtedly lower, levels of
benzo-type drugs (including illicit market, novel psychoactives, and similar
prescribed drugs) means overall use is probably increasing. Workers have
reported people entering treatment with staggeringly high levels of
benzodiazepine dependency, built up exclusively using street benzos.
Benzos are used recreationally in a
number of settings. Alcohol and benzos areused together to enhance and increase
intoxication. Some stimulant users take benzodiazepines to alleviate the
"come-down" from speed, Ecstasy or cocaine, and to promote sleep.
It is not uncommon for dependent heroin users to use benzodiazepines when
heroin is unavailable, or low quality. It is also used to help offset some of
the symptoms of withdrawal. The use of benzos on top of prescribed opiates -
such as with methadone or Subutex - is also common as it can make the effects
of the opiates feel stronger. Such use increases risk of overdose.
Many people self-medicate with benzodiazepines to alleviate mental discomfort
caused by mental health problems, painful memories, or to escape unpleasant
circumstances. For such users, where unsupervised use may be long-term and
extensive, careful assessment of needs, of underlying reason for the drug use,
and comprehensive care plans are likely to be needed to achieve reduction and
cessation of drug use.
 This
work is licensed under a Creative
Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
This
work is licensed under a Creative
Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Kevin
Flemen/KFx: this version 08/22
Drug Facts: