Fact Sheet (PDF) | Facts Card: Image or PDF | Harm-reduction information: Image or PDF | Links | Resources
AKA: booze,
bevvie, juice, sauce, alcopops, beer, wines, spirits. There are
numerous forms of alcohol. The alcohol found in alcoholic beverages is ethyl
alcohol (ethanol). Other forms include methyl alcohol (methanol) which is
highly toxic.
Source: Alcohol is produced as yeast
metabolizes sugar. Grains, fruit or vegetables are fermented and the resulting liquid
drunk, or the alcohol extracted by distillation for further processing.
Alcohol
is sold via licensed outlets such as supermarkets, off licenses and bars.it is
also brewed at home and in custodial settings.
Appearance: Ethanol is a clear liquid with a
distinctive smell. Vodka is effectively ethanol further diluted with water and
no other additives. Other drinks will contain colour and flavour from the
original source material, the brewing and fermenting process or added after
fermentation. For example wine colour comes from the skin of grapes, the colour
of whiskey is from the material through which it is filtered and barrels used
for fermentation and alcopops are the result of sugar, colour and flavours
added post-fermentation.
Costs: Alcoholic drinks range in price
from under £1 for cheap lagers through to many thousands for expensive wine. In
Scotland a “minimum unit price” of 50p per unit was introduced to address the
provision of super strength lagers and ciders.
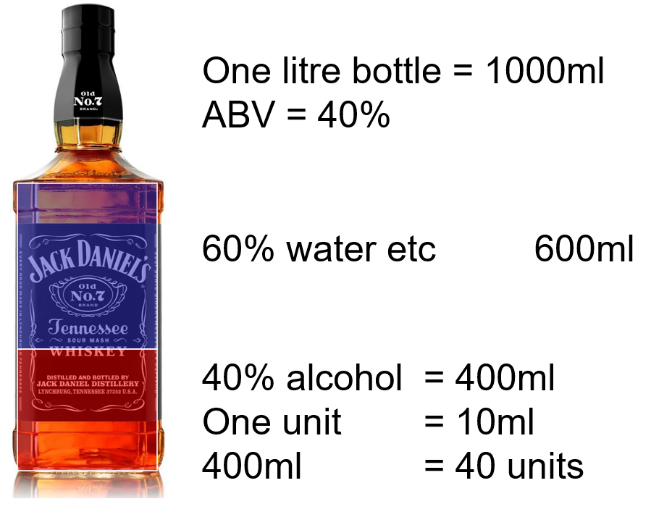 Strength: Alcohol strength is measured as
ABV (alcohol by volume), the percentage of alcohol in a drink. A 1litre bottle
(1000ml) at 40% ABV contains 400ml of ethanol and 600ml of water and other
additives.
Strength: Alcohol strength is measured as
ABV (alcohol by volume), the percentage of alcohol in a drink. A 1litre bottle
(1000ml) at 40% ABV contains 400ml of ethanol and 600ml of water and other
additives.
The older term “proof” is no longer used in the UK. It was based on the fact that
drinks of around 50% ABV would ignite and burn away. This was the Proof – that
the drinks had an ABV of 50% or more. This would be referred to as 100 proof.
Drinks with less than 50% would not ignite – underproof.
Alcohol is also counted in UNITS. A UNIT of alcohol is 10ml of pure ethanol or
7g. Some drink producers state the number of units on the packaging but this is
not always the case.
When trying to calculate units there are a number of tools and apps such as
“Drink Wheel,” and Unit Counter tools to help.
The easiest way to work out the units in a drink is:
volume (in litres) x strength
(the ABV:
e.g. a bottle of wine: 0 75 (litres) x 13 (ABV) = 9.75 units
In
practice the number of units quoted in a drink is an approximate figure based
on the approximate size of the drink and the ABV, usually rounded up. The
figures below look at the most common drinks. Where a person is pouring or
mixing their own drinks, it becomes much harder to accurately count units
|
Product |
ABV(%) |
Volume |
Units (approx) |
|
Wine |
12% |
Standard Glass (125mls) |
1.5 Units |
|
|
13% |
Bottle (750mls) |
10 Units |
|
Spirits |
37.5% |
25ml (small single) |
.9 Unit |
|
|
40% |
35ml (large single) |
1.4 Units |
|
Alcopops |
5.5% |
275ml |
1.5 Units |
|
Beer |
3% |
1 Pint |
2 Units |
|
Cider |
5% 8.5% |
1 Pint |
2.8 Units |
Purity: Professionally produced drinks are
not simply alcohol + flavour. They can contain a number of other chemicals some
of which may be psychoactive and others which could cause adverse reactions.
Some people are, for example, intolerant of tannins found in some wines and
spirits, and the congeners which give dark spirits their flavour and colour can
be unpleasant too.
Chemicals such as GHB naturally occur in some wines.
Illicitly produced alcohol may contain more dangerous contaminants. Illicity
brewed and bootleg alcohol may contain dangerously high levels of methanol
which breaks down to form the toxin formaldehyde. Buying bootleg alcohol or
badly-made hooch can be dangerous and potentially life-threatening.
Safe(r) Drinking Limits:
There
aren’t really any safe drinking levels and medical consensus is that for most
of the population all alcohol use is damaging, and the safest approach is
simply not to drink.
However levels of drinking are associated with different levels of risk and the
Government guidance is for those who do drink to reduce risk by drinking at levels
associated with a lower level of harm.
In the
past drinking levels were presented as number of units per week with different
levels for men and women. This saw people who may have been drinking within the
“safe” weekly levels but were drinking harmful amounts over a small number of
days. To address the safer level guidance is presented in terms of units per
day and per week. Medical evidence no longer supports the different levels for
men and women so this difference has been removed from the guidance.
So the
current drink levels for men and women are:
|
2-3
units a day or less: |
14-21
units/week |
no
significant risks |
|
3-5 units per day: |
21-35 units/week |
moderate risk |
|
5+ per day |
35+/week |
high risk |
Patterns of use: Both
constant drinking and binge drinking are unhealthy. It is safer to aim for at
least two alcohol-free days per week; a person who is finding it difficult to
achieve this may want to seek assistance to moderate their drinking.
Binge
drinking (more than eight units for men and six units for women is a UK
interpretation) is associated with heart and circulatory problems such as high
blood pressure.
The Liver and Units of
Alcohol:
Ethanol is broken down by the liver in several stages using enzymes.
Ethanol >>> alcohol dehydrogenase (ADH)
>>> acetaldehyde
acetaldehyde >>> aldehyde dehydrogenase (ALDH) >>> acetic
acid
Acetaldehyde is highly toxic and responsible for some of the
unpleasant symptoms during and after drinking. Some people can’t produce the
enzyme ALDH so can’t break down acetaldehyde making them “alcohol intolerant.”
The liver
of an average healthy male can remove approximately one unit of alcohol from
the blood stream. While this alcohol is being metabolised, the rest remains in
circulation. This means that if, between 8 and 12pm a person drank two bottles
of wine, it would take at least twenty hours for all the alcohol to be
metabolised out. By the time we factor in the time for alcohol to be absorbed,
when drinking commenced and ended and a reduction in liver enzymes needed to
break down alcohol the length of time will in practice be longer for a lot of
people.
Drinkers may well have excessive levels of alcohol in the blood-stream the day
after a heavy nights drinking.
Women,
people with impaired liver function and people of small build will generally
metabolise alcohol more slowly, get drunk faster and sober up more slowly.
Women may also find that tolerance to alcohol decreases during just prior to
the start of menstruation.
Methods of Use: Alcohol is usually drunk; it is also eaten and used
in cooking. When heated, most alcohol is evaporated away; however, alcohol can
be eaten in cold products such as jelly.
Alcohol
is also sometimes used in other ways such as via snorting it, injecting it or
attempting to absorb it via the eye. These methods are invariable painful, and
while young people may attempt to snort alcohol or eyeball it, such efforts are
rarely pursued. Recently, companies have tried to promote 'alcohol with oxygen'
a machine that allows alcohol to be breathed in via a face mask and absorbed in
the lungs. Such a method means that alcohol initially bypasses the stomach and
the liver, so gets intoxicated more quickly. However, such equipment in bars
falls foul of licensing laws and so has not become more widespread.
Alcohol
can be absorbed through other mucous membranes – such as an alcohol enema – but
this is (a) not that common (b) messy (c) can cause overdose.
Injecting
alcohol is quite unusual. It is most often injectors habituated on injecting
processes who may attempt this painful activity.
Effects: Onset of
alcohol will depend on the strength of the drink, previous food intake, other
substances used and the user's general build and metabolism.
Alcohol
is primarily a depressant drug - making the person drowsier and moving them
towards sleep and unconsciousness. It does this by mimicking the brain chemical
GABA, which
reduces electrical signals in the brain and body.
However,
early on it can act as a euphoriant, elevating levels of the brain chemicals serotonin and dopamine.
This makes the person more animated, lively and talkative. As more alcohol is
taken in, the depressant effects can become more marked as reactions and
muscular control are impeded.
At higher
doses, the drinker may become drowsier, with slurred speech, difficulty standing
and stupor. Finally, the person may become unconscious.
People
experience a wide range of different moods when drinking; some people describe
feeling happier, while others become less happy and more withdrawn; others may
become aggressive. To some extent, alcohol may act as a mood amplifier,
exacerbating a mood or state that was already there. Others would argue that
alcohol reveals underlying personality traits, and the rest argue that
different drinks affect people in different ways.
Alcohol
can also cause nausea, vomiting, excessive urination, impaired memory and
judgement.
Many
alcohol users will be familiar with the 'hangover' which is a symptom of
excessive alcohol use. The symptoms tend to include nausea, aches in the lower
back, headaches, sensitivity to light and sound and a general sense of feeling
unwell. These symptoms result from high levels of dehydration, brain chemistry
adjusting to absence of alcohol, irritation of stomach, swelling of the liver
and removal of toxins from the blood.
Health Implications: There is
no commonly used drug which is more toxic to more parts of the body than
alcohol. Excessive use of alcohol can have a devastating impact on health.
Alcohol-related
harm could directly affect the user or other people indirectly affected. Harm
takes place in the short, medium and long term.
Short term risks:
Risk taking behaviour: because alcohol disinhibits it can lead to
impaired decision making This could lead to other risky behaviours including
episodes of unplanned drug taking, unsafe sex, fights, offending or other risk
taking. It also increase the risk of lapse for people endeavouring to abstain
from drug use.
Alcohol poisoning: Drinking too much can also lead to alcohol
poisoning, which can be fatal, and according to the National Drugs Helpline,
over 1,000 people under the age of 15 are admitted to hospital each year with
alcoholic poisoning and all require emergency treatment.
The risks
of dangerous alcohol overdose is increased by mixing alcohol with other drugs.
Key risks come from mixing alcohol with stimulants (such as cocaine) which
allow people to drink larger amounts in the short term, but leave the person
dangerously intoxicated once stimulants have worn off. The combination forms a
new psychoactive compound cocaethylene which is longer acting
than cocaine, but more liver and cardio-toxic.
The other
key risks come from mixing alcohol with sedating drugs, especially opiates and
benzodiazepines. The combined effect of alcohol with these drugs significantly
increases the risk of fatality.
Binge
drinking can also lead to irregular heartbeat and acute pancreatitis.
Medium
term:
Excessive
alcohol use in the medium term is associated with:
Long term
Long term excessive alcohol use is associated with significant damage to many
organs:
Alcohol
is directly associated with between 50-70,000 deaths per year.
Alcohol and pregnancy: Alcohol use during pregnancy can damage the foetus
and this leads to a range of physical and developmental issues referred to by
the umbrella term Foetal Alcohol Spectrum Disorder.
For
managed, women who are non-dependent drinkers who are pregnant or seeking to
become pregnant, the (conflicted) advice is to abstain from alcohol or limit it
to one to two units per week to minimise risk of harm.
For women
with alcohol problems including dependency, discussion about effective
contraception is important. Heavy alcohol use can mask early indicators of
pregnancy but once a pregnancy is identified it is important to support
engagement with alcohol and midwifery services so risks can be minimised.
Indirect risks: Alcohol is also a key factor in many social and
industrial accidents, road traffic accidents and homicides. It is a significant
aggravating factor in assaults and domestic violence and a feature of much
offending.
Alcohol and Mental Health:
Alcohol
has a complex relationship with mental wellbeing.
Alcohol and depression: In the short-term alcohol elevates dopamine and
serotonin and so can alleviate symptoms of depression. Some people may end up
using alcohol to self-medicate for existing low mood.
As alcohol mimics GABA it can increase relaxation and drowsiness and so gets
used to reduce anxiety and help with sleep.
With longer term and heavier use, alcohol will start to damage stomach and guts
which can inhibit the production of serotonin and dopamine. These brain
chemicals are being used up faster than they can be replenished and diet may
suffer as money is spent on alcohol rather than quality food. These factors can
result in lower levels of dopamine and serotonin causing or increasing
depression.
The risk is now that alcohol use will be used in the first instance to help the
person feel happier (which won’t work as alcohol can’t replace the missing
dopamine/serotonin) and then just to blank out the low mood.
In other words early drinking may have been to feel better and later drinking
is just not to feel. Or early drinking was for pleasure and later drinking to
avoid “displeasure.”
Too
frequently antidepressants are prescribed to people drinking excessively and
experiencing depression in the hope or mistaken belief that these will
alleviate depression and therefore positively impact on alcohol use. In truth,
beyond placebo effect such an intervention is unlikely to be effective.
Cessation of alcohol, healing of the gastro-intestinal track, diet improvement
and other holistic interventions will be essential at which point
antidepressants could be a useful adjunct.
Alcohol and anxiety: Alcohol was also mimicking the effects of GABA and
with excessive drinking the brain starts to adapt, over-producing GABA’s
“opposite number” Glutamate, and producing less GABA. These higher levels of
glutamate and lower levels of GABA can increase anxiety and stress and so
again, alcohol use which have once been to help manage anxiety now increases to
manage the anxiety resulting from excess alcohol use.
Alcohol and psychosis: Alcohol causes dopamine and serotonin levels to go
up and can interfere with anti-psychotic medications so drinking for people
with a psychotic disorder can cause more symptoms, disengagement from
medication and disinhibited behaviour which increases risk of people acting on
impulse.
This also applies where people are having suicidal thoughts. Alcohol can worsen
depression, increasing risk of suicidal thoughts. And alcohol can disinhibit,
increasing the risk that the person will act on these thoughts.
Heavy
long term use of alcohol can cause alcohol-induced psychosis, a state of
delusion, panic and disordered thinking which increased with alcohol
consumption and should start to reduce as alcohol use is reduced.
Long term excessive drinking can cause organic brain damage under the umbrella
term “Alcohol-related Brain Damage.” This can include dementia, impulsive
behaviours, memory and balance problems. The most commonly referred to
diagnoses are Wernicke’s Encephalopathy and Korsakoff’s Psychosis.
Alcohol and Dependency:
Alcohol
use can lead to physical and psychological dependency. Alcohol dependency is
often not assessed properly as there are some common erroneous assumptions such
as that dependent drinkers will go into withdrawal without a drink, or that
they will be drinking in the morning or drinking daily. Not all dependent drinkers
are physically dependent. The clinical definition of Alcohol Use Disorder
was revised in DSM V (the Diagnostic and Statistical Manual used extensively by
American Psychiatrists) and changed from having separate “alcohol misuse” and
“alcohol dependency” categories. You can read more about how it changed here
here:
Rather
than just thinking about physical dependency we are looking at a collection of
indicators including:
·
Difficulty with control
·
Evidence of harm (physical, psychological, social,
situational)
·
Escalation
·
Physical withdrawal symptoms
·
Psychological withdrawal symptoms
·
Alcohol as a priority
·
Individual or others expressing concern
UK Clinicians
will often use a short standardised screening tool such as AUDIT https://auditscreen.org/ to assess for alcohol dependency
but failure to interpret AUDIT correctly or an unwillingness for a person to
answer questions openly can mean problematic or dependent drinking can go
unidentified.
Drink diaries are tools used to help assess, monitor and promote change in
drinking behaviours. They are sometimes derided as being of no use with heavy
drinkers and only really useful with moderate and excessive drinkers who can
control their drinking but a well completed drink diary can be a very useful
tool in all aspects of drink management.
There are
simple drink diaries, paper versions, online ones and apps. However there are
some specific things that we should be looking for in a good drink diary:
|
Date |
What I drank |
How much (units) |
Time/Place |
How I felt before |
How I felt during |
How I felt after |
Other notes |
|
|
|
|
|
|
|
|
|
Drink diary and the cycle of change:
Lots of
people starting to engage with a service are at best contemplative about
addressing their drinking. Many aren’t seriously contemplating change – they
may have been referred by someone else and don’t see their drink as a problem.
-
A willingness to start to complete a drink diary is
a very first step to exploring the issue of “do I drink too much.” Which
is the start of a journey towards contemplation.
-
Some people will already subconsciously be aware
that they are drinking a lot; by noting it down and adding it up they can make
this much more concrete – the “wow, that’s a lot and I didn’t think it was
that much” can help recognise unhealthy drinking
-
In terms of pros and cons work the
before/during/after sections can help unpick some of the conflicted feelings
around alcohol. I may say I help to drink with low mood but I can see from my
diary that I am often low after drinking which helps me revisit pros and cons
of drinking.
The
language of drinking pathology is deeply unhelpful and creates barriers to
change. We talk variously about:
- alcohol dependency
- alcohol use disorder
- alcohol addiction
- alcoholism
Each of these have different meanings from professionals, people who drink and
wider society. And they each bring with them their own barriers. So people may
for example say “I’m not an alcoholic.” This is in part because the term
is laden with social meaning (down and out, strong lager, drinking in the park,
red nose), treatment meanings (12 steps, higher powers, addiction, disease) and
consequential meaning (can never have another drink.) So the person may refuse
the label and in turn refuse to acknowledge the issue.
So rather
than using these labels less confrontational approaches can help.
For example a workers could ask “on a spectrum from healthy to very
unhealthy, where would you put your relationship with alcohol over the last
year.” A person may find it easier to acknowledge that they have an “unhealthy
relationship with alcohol” as it’s not got the same baggage attached to it
as some of the other terms.
One of
the other key challenges is lots of people come in to contact with services at
a point where they may want to drink differently but aren’t currently looking
at stopping completely. Abstinence is a huge and challenging step. We live in
an alcohol-suffused society where the ability to drink, drink happily and drink
“responsibly” are part of the social norms. Stopping drinking is to drop out
from a huge part of UK social culture and is a threatening step to contemplate.
As a
stepping stone we may want to explore managed drinking and control first. In
doing so we might also help the person identify that, actually, they need to
stop drinking.
A
motivational conversation could look like this:
A is the
person who drinks; B is the person offering support.
|
A: I don’t have a problem with my drinking; it’s under control |
This conversation uses elements of motivational interviewing and establishing a
SMART target. Importantly it’s A’s target of 50, not B’s. B doesn’t state that
it’s unhealthy to drink at 100 units per week but reinforces and amplifies A’s
own statements about this.
The drop from 100 to 50 still leaves risk of alcohol related harm BUT it needs
to be A’s target so they own it. At the end we have a specific
time-bound target to work towards.
B can then
explore alcohol management strategies to get this target. This is the journey
from precontemplation to action.
It could be successful and result in a drop in alcohol consumption. This can
demonstrate the capacity for self-management and control. And if A do a journey
from 100 to 50 they can also see that they can do 50 to 25. A has the capacity
to be a managed drinker and through engagement with B has developed the
motivation and tools to achieve this.
Alternatively
the attempt may not work and there’s no reduction in alcohol use. This approach
may be attempted a few times, with different approaches and targets. But it can
help the person come to terms that despite their best efforts they struggle to
manage their alcohol use and abstaining may be the best option for them.
We might then
need to explore cessation strategies.
Alcohol dependency and
withdrawal:
Dependency on alcohol is far more than the physical aspects of withdrawal. It
includes the drivers for drinking, the perceived benefits of drinking, social
and ritual aspects of alcohol use, fears or withdrawing, practical difficulties
in withdrawing, and learning to live without alcohol.
Cues and Craving: Alcohol is (especially early on) a dopaminergic
drug giving feelings of reward and euphoria. So regular drinking builds up an
association with alcohol being a reward. The associated cues (time of day,
places, people, tastes, moods) cause dopamine release leading to anticipation
and craving and motivating the person towards drinking which in turn causes
further dopamine release and reward.
As
dopamine levels drop the urge to redose will kick in, encouraging further
drinking.
Simultaneously
alcohol is mimicking the effects of GABA reducing activity in decision-making
areas of the brain. This means that my determination to only have one drink is
undermined by two things: my dopamine-induced craving for another drink and my
disinhibition from reduced activity in the Prefrontal Cortex making it less
likely I’ll say no to the second drink.
This is part
of alcohol dependency – about the triggers and cues and disinhibition that lead
to unmoderated drinking.
Tolerance and neuro-adaptation: Regular use leads to tolerance
where more alcohol is required to achieve intoxication. This leads to changes
in brain chemistry and changes to structures in the brain.
With regular and frequent drinking:
- the brain makes less GABA as alcohol is doing the job of GABA
- the brain makes more Gutamate (GABA’s opposite number) to try and get brain
activity back to normal.
As a result of this more alcohol is needed to achieve intoxication and keep the
excess Glutamate in check.
In response the brain continues to adapt, less GABA production and less GABA
receptors and more Glutamate production and increased sensitivity to Glutamate.
At this point the person needs large amounts of alcohol to avoid the symptoms
of all this excess glutamate.
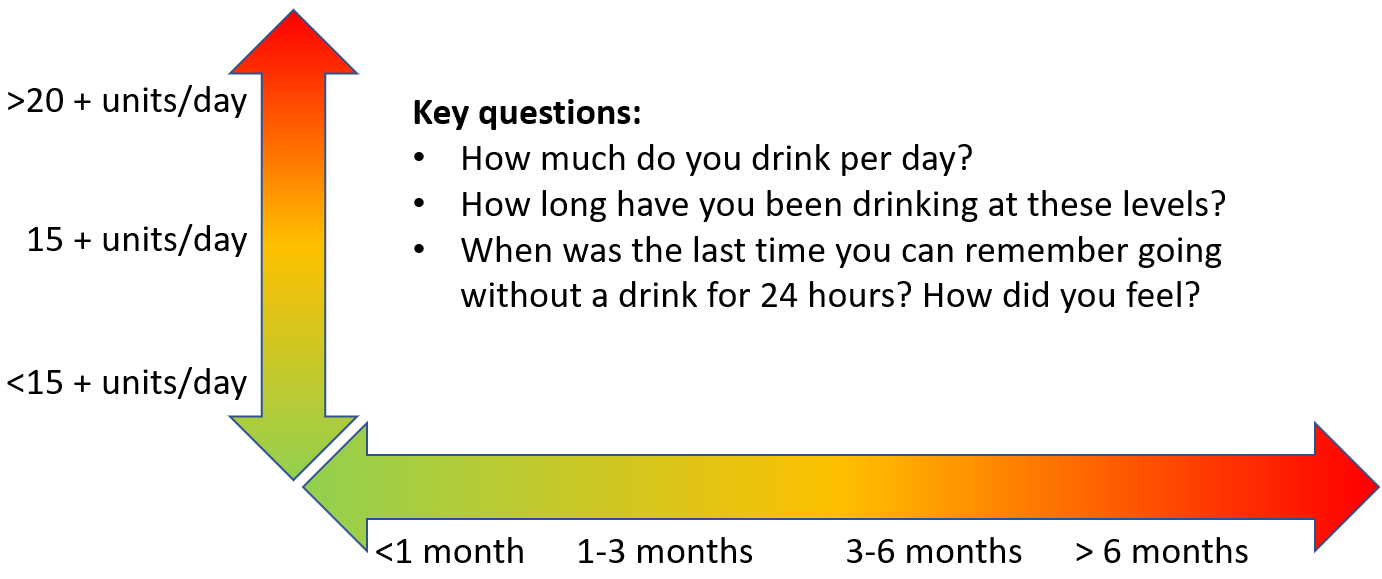
For
people drinking at a rate of 10 units or less per day there’s plenty of time
for all the alcohol to clear from the body and the brain chemistry to get back
to normal. But as alcohol use increases there’s less and less time for the body
to detox each day. At the 15-unit mark there’s barely enough time for all the
alcohol to clear and brain chemistry to rebalance. And if we consume more than
20 units then there’s always alcohol in the body and the brain can not get back
to normal before more alcohol arrives.
Again, this
is one of the areas where a good drink diary is helpful. It can help to
establish who is likely to be at risk of physical withdrawal symptoms.
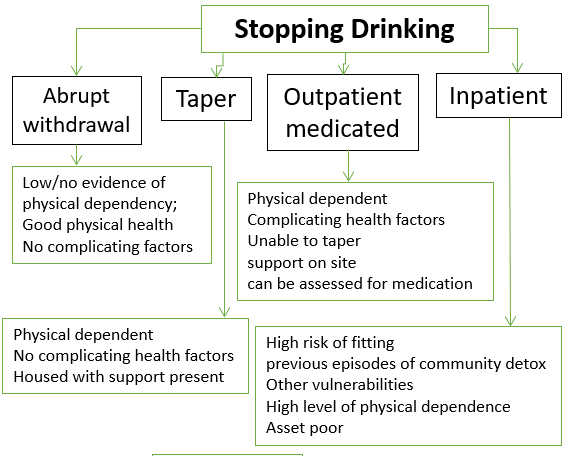
For
people at the lower end of the risk spectrum (lower levels of use for shorter
periods of time) with good physical and mental health, motivated and with
support, it is feasible to stop alcohol abruptly and with no withdrawal risks.
Alcohol Withdrawal:
Where
there is a risk of physical dependency on alcohol then stopping suddenly can be
dangerous leading to significant physical and psychological risks. This an
include seizures, convulsions, hallucinations and psychosis. It can be
distressing and has the potential to cause permanent harm or be fatal.
Risk of
withdrawal is increased if the person has underlying health issues that could
be worsened by withdrawal (mental illness, convulsions) or has experienced
withdrawal symptoms in the past (a process known as “kindling” where the
likelihood of severe symptoms appears to increase if there has been previous
bad withdrawals.
For
people who cannot stop abruptly options are:
·
Stop by tapering of alcohol
·
Stop alcohol and manage symptoms in the community
or on a ward with medication
Tapering is where the person reduces their alcohol consumption by around 25% a
week until they can stop completely. It is best for people living in the
community with professional or peer support and is not suitable for people with
underlying health conditions or living without support.
Medicated detoxes usually involve the benzodiazepine chlordiazepoxide (Librium)
which is used to reduce withdrawal symptoms such as convulsions, panic and
insomnia. It is dangerous if used with alcohol so the person needs to stop
drinking and then start using Librium as withdrawal symptoms start to emerge.
Should drinking resume then they need to step away using Librium which could
otherwise cause a fatal overdose. In the community people detoxing with Librium
should be housed with support on site to manage a lapse while prescribed.
Post-acute withdrawal: The brain can take a long time to
get back to “normal” after the acute detox period. With glutamate levels too
high and GABA levels still low the person may continue to experience anxiety
and jitters for weeks or months after.
The drug Acamprosate is often prescribed to help manage these symptoms
alongside psycho-social interventions.
As discussed earlier, alcohol will have caused low levels of dopamine and
serotonin and once the person is sober they are likely not just to experience
low mood but be much more aware of their low mood and other emotions that were
previously being blocked by alcohol.
There may, for some people, be a role for anti-depressant prescribing if very
low mood is jeopardising recovery. But this should be alongside other
psychosocial and holistic interventions so that antidepressants can be a short
term intervention to help promote and sustain change.
Withdrawal from alcohol can be physically and mentally difficult; given its
high social acceptance, remains a hard drug to avoid in daily life. It can
cause serious physical symptoms in withdrawal.
In order to initiate and sustain a range of interventions can be useful
including counselling, therapy, trauma work, and group work can be useful.
A key source of support for people looking to address their alcohol use is AA
(Alcoholics Anonymous).
 Screening:
Screening:
Standard
screening tools such as AUDIT are routinely used in alcohol services and there
are additionally “12 questions” which are in the Alcohol Change “Blue Light
Toolkit” which are useful.
The questions below can help generic workers and drug/alcohol workers identify
issues relating to alcohol related risk and harm.
|
Screen for |
Explore |
|
Is use
stable or escalating |
Marker
for situation deteriorating or tolerance building |
|
What
brings your drinking episodes to an end? |
Looks
at do you control it, someone else has an influence or only stops because you
are stopped from drinking by lack of money, health, arrest etc |
|
Do you
use alcohol with other substances |
OD
risk, education re cocaine/alcohol & benzos or opiates + alcohol |
|
Have
you done things when you’ve been drinking that have shocked you or you’ve
been distressed by when you were sober |
Looks
at risks in relation to disinhibited behaviour |
|
Where
are you drinking? |
Looks
at dangerous drinking environments or risky company when drinking? |
|
Could
you be pregnant? How effectively are you using contraception? |
Look at
issues around pregnancy and safe sex. |
|
Have
you found yourself gaining weight |
Alcohol
is calorific and can contribute to weight gain |
|
When
did you last have blood pressure checked? |
Heavy drinking
can contribute to weight gain |
|
Do you
find yourself with stomach pains or burning in stomach? |
Heavy
drinking can cause and worsen stomach problems |
|
Have
you had your liver function checked |
If not
can identify symptoms of fatty liver or early evidence of inflamed liver |
|
Do you
find you are getting bruises |
Could
be a marker for liver problems, vitamin deficiency or possibly abuse |
|
Have
you noticed any yellowing of eyes or skin |
Marker
for liver problems |
|
Do you
find yourself getting more itchy skin |
Marker
for liver problems but could also be a marker for neglect |
|
Have
you found that your poo is more greasy or your urine has got darker in colour |
Markers
for liver problems |
|
Have
you found yourself being sick? |
Marker
for gastritis |
|
Do you
find yourself with symptoms like heartburn or reflux |
Could
be hiatus hernia or damage to pyloric sphincter muscle |
|
Have
you found blood on your poo |
Marker
for intestinal bleeding – could be colitis or indicator of bowel cancer |
|
Any
evidence of swelling to the belly |
Indicator
of ascites – fluid from liver accumulating in the abdomen |
|
Have
you been falling more |
Balance
problems could be a sign of brain damage or possible numbness at extremities |
|
Have
you suddenly started to lose weight |
Could
be that the liver is struggling to synthesis glucose and person is burning
fat and muscle as a result (ketosis) |
|
Is
there a smell of acetone on breath? |
Indicator
of ketosis and marker of serious malnutrition/liver problems |
|
Any
smell of urine or faeces? |
Marker
for incontinence or possible neglect |
|
Have
you found it harder to remember people’s names, recent conversations or
things you meant to do? |
Start
to screen for possible memory deficits which could be early indicators for
brain damage |
|
How
well do you think you are coping at the moment? |
Screening
for low mood, very poor mental health |
|
Apart
from this conversation where else can you go for support about your drinking |
Looking
at strategies for support and reduce isolation |
LEGAL STATUS: Alcohol is covered by licensing
laws and other regulations as follows:
·
Under 5: It is illegal to give alcohol to a child
under five years old in any circumstances excepting on the orders of a doctor.
·
5+: It is legal for children over the age of five
to drink alcohol on private premises, such as in the home.
·
14+: Young people between the ages of fourteen and
seventeen may be in a bar during opening hours but may not buy, be bought or
drink alcohol on the premises.
·
16+: Young people sixteen and seventeen years of
age may buy or be bought certain drinks in licensed premises but only in a separate
eating area and only for consumption with a meal. The permitted drinks in
England and Wales are beer, cider and perry. In Scotland, they may also
purchase and consume wine with the meal.
·
Under 18: It is illegal for any person under
eighteen years of age to buy any alcohol from an off licence, attempt to buy
alcohol or for someone else to buy it in order to supply it to someone under
the age of 18.
·
Confiscation of Alcohol (young Persons) Act 1997:
·
Empowers police to require under 18-s to hand over
alcohol in a public place. Failure to do so (without reasonable cause) and give
name and address when requested summary offence and carries power of arrest.
Other
·
Local by-laws re. Public drinking; many areas
prohibit this and this can lead to a fine.
·
Drunk and disorderly, Drink driving, Drunk in
charge of a vehicle.
OTHER INFORMATION: Alcohol is a widely used drug. Its legality and social acceptability mean that we don’t always talk about it as much as we could or should. However, it is one of the most important drugs that we need to engage with, causing huge levels of harm to individuals and wider society. Informed, high quality interventions around alcohol are a critical aspect of any drugs work.
Drug Facts: